Your heart sinks into the pit of your stomach, your hands are tied and you’re struggling to find the words to express how you’re feeling. That’s because you’ve just learned that someone whom you care about deeply is being hurt in some way by their significant other—and you’re not sure how to help them. You’re overcome with paralyzing grief and disbelief.
Whether the inflicted pain is emotional, financial, physical, psychological (e.g. stalking) or sexual, this pattern of behavior is abuse. When abuse happens between individuals in intimate relationships or those who live in the same home, it’s classified as domestic violence.
“Abuse is all about power and control,” said Dr. Kimberly Vess Loomer, the associate dean for student and multicultural affairs at Augusta University. “It’s a public health issue, because it affects overall health and permeates every culture and socioeconomic status—every walk of life. Domestic violence, in particular, affects entire families.”
In her role, Loomer teaches a cultural competence class for first-year medical students so they can be aware of the signs of domestic violence. This allows them to prevent and treat it as quickly as possible.
“This is important for our patients,” Loomer said, “because they can rest assured that they’re being treated in an environment where our physicians are skilled at recognizing when they need our help.”
Signs of domestic violence
If someone is suffering domestic violence, he or she may show physical and psychological signs, which are as follows:
- Direct physical signs: Bruises, frequent injuries that have a hard-to-believe cause
- Indirect physical signs: Weight gain, tobacco use, substance abuse
- Psychological signs: Isolating oneself and being withdrawn from relationships, suddenly more depressed or anxious than usual
Sound like something you’ve seen before? The good news is that there are things you can do to help while protecting yourself.
1. Share your concern with them without judgment.
Express your concern in a delicate, supportive way: “I’ve noticed that you’ve been distant lately. I miss you. Is everything OK?” Or, “I’ve noticed that you seem to have a lot of injuries these days; do you want to talk about it?”
2. Support their choices.
“On average, a person will leave his or her abuser seven times before permanently leaving,” Loomer said, “so it’s important to keep in mind and respect that the person you care about may not take action as swiftly as you’d like them to.”
That’s because there are several barriers to leaving that cause the abused person to second guess whether they should leave. They are as follows:
- They lack the resources necessary (or that they feel are necessary) to go out on their own. This is especially true for those who are victims of financial abuse.
- They may be fearful for their life or the lives of their loved ones.
- They want to keep their families together.
- Their personal beliefs regarding marriage and divorce, gender roles, etc. outweigh their motivation to leave.
3. Encourage them to maintain relationships outside of their intimate partner relationship.
You very well may be the abused person’s only link they have to outside relationships. While your role in their life is critical, you can’t do it alone, so encourage that this person to maintain other relationships.
4. Encourage them to develop a plan.
If the abused person needs to leave their home, encourage them to develop a plan. This includes collecting the necessary documentation they’ll want to take with them (e.g. children’s social security cards and birth certificates, financial resources, a phone to which the abuser doesn’t have access, etc.).
“Remember, abuse is about control,” Loomer said. “If the abused person leaves without these things, he or she may not get them back. Regardless, health and safety is of utmost importance. Things can be replaced—people cannot.”
5. Play it safe.
Do not let the abuser know that you know about the abuse, because that could escalate the situation and not only make it worse for the abused person but could also make you a target.
6. Assist in any way you can.
This can include offering transportation, care for children or a place to stay.
“This part of the phase can be very exhausting,” Loomer cautioned. “Again, it takes seven attempts for someone to leave his or her abuser, so keep in mind that if you choose to support the abused person, prepare to be in it for the long haul.”
As with anything, the best advice is to maintain healthy boundaries.





Misinformation about DV abounds.
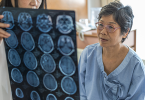
1. Because most blows are to the head and face, abused women sustain more concussions than NFL football players and yet professionals consistently fail to have women tested for brain injury.
2. Abused women need to donate our brains to science for study.
3. A reason women may be unable to leave that is consistently omitted from the list, is that brain injury contributes to poor decision making and planning. Women may be able to make a plan and not be able to follow through.
4. Awareness is on a continuum and many women are clear that they are NOT to blame for other people’s choice to use violence.
5. Being a victim of violence (an experience) does not render women “mentally ill”. ‘MI’ is a social construct per the biological medical model, and is not a bona fide medical disease.
6. Psychiatric drugs are contraindicated and unapproved for use in vulnerable brain injury survivors because they have been known for over 40 years to cause brain injury. (Breggin)
7. The standards of practice and the DSM prohibit labeling and pathologizing victims of “family violence” which both causes more problems for victims and allows the focus on the abusers to be diverted.
8. The only thing that has ever been successful in curbing violence is swift, predictable consequences.
9. The failure of the court system to support women seeking damages for the torts, costs, loses, hardships and disability they suffer at the hands of their abusers, perpetuates abuse against women and girls.
10. Access to justice is a Me too issue. #@2J #METOO
©JMGayton 10/8/2018 MH,AB,CA